
Infection inside of the uterus during pregnancy (chorioamnionitis).Early rupture of membranes, which causes leaking amniotic fluid before the end of pregnancy.A fall or other type of blow to the abdomen.Hypertension-related problems during pregnancy, including preeclampsia, HELLP syndrome or eclampsia.Chronic high blood pressure (hypertension).

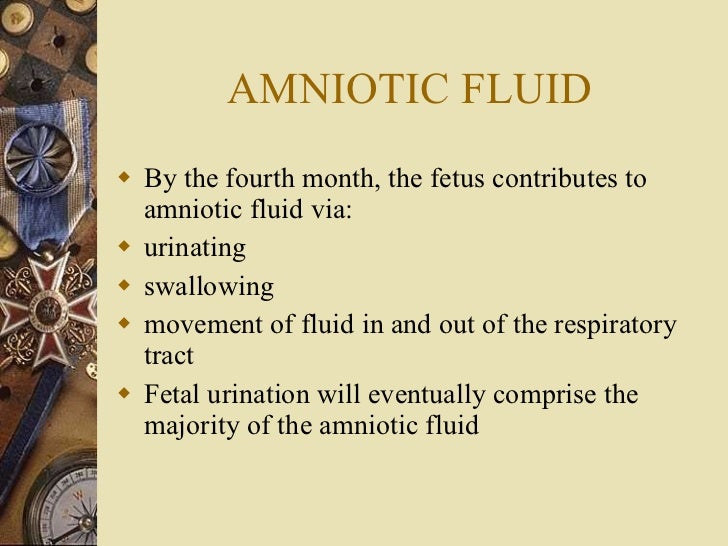
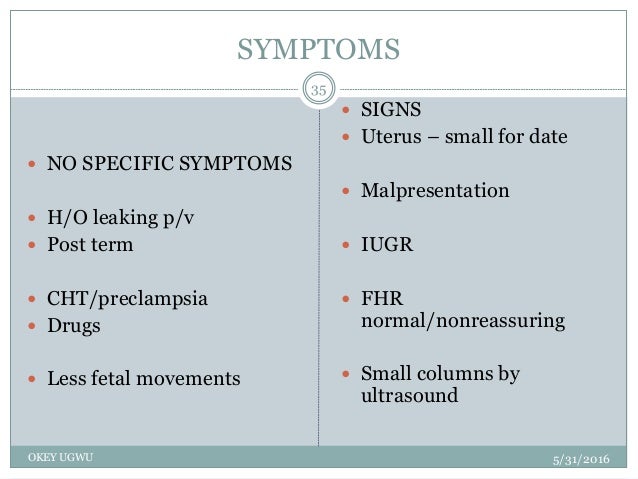
 Placental abruption in a previous pregnancy that wasn't caused by abdominal trauma. Risk factorsįactors that can increase the risk of placental abruption include: Possible causes include trauma or injury to the abdomen - from an auto accident or fall, for example - or rapid loss of the fluid that surrounds and cushions the baby in the uterus (amniotic fluid). The cause of placental abruption is often unknown. Seek emergency care if you have signs or symptoms of placental abruption. Your baby might not grow as quickly as expected, and you might have low amniotic fluid or other complications. In some cases, placental abruption develops slowly (chronic abruption), which can cause light, intermittent vaginal bleeding. It's possible for the blood to become trapped inside the uterus, so even with a severe placental abruption, there might be no visible bleeding. The amount of vaginal bleeding can vary greatly, and doesn't necessarily indicate how much of the placenta has separated from the uterus. Uterine contractions, often coming one right after anotherĪbdominal pain and back pain often begin suddenly. Vaginal bleeding, although there might not be any. Signs and symptoms of placental abruption include: This study also included RCTs published after the most recent amendment to the Cochrane review.Placental abruption is most likely to occur in the last trimester of pregnancy, especially in the last few weeks before birth. In the other review, 2 the inclusion criteria were limited strictly to studies in which induction was initiated at 41 weeks' gestation or later. The benefit of induction was found in studies in which induction occurred after 41 weeks. Trials included in the Cochrane review 13 fell into two main groups: those in which women were recruited at or before 40 weeks' gestation and those in which recruitment occurred at 41 or 42 weeks' gestation. The primary difference between the meta-analyses was in the studies chosen for inclusion. In both reviews, the largest single RCT was the CMPPT (3,407 patients) the next largest individual RCT included 440 women. In neither review did an “unfavorable” cervix at the time of induction result in increased rates of cesarean delivery or other adverse outcomes. Neither review 2, 13 found any adverse perinatal complications from labor induction, and both noted that the results were consistent regardless of the Bishop score at the time of induction. No differences were found in neonatal morbidity outcomes. No difference was found in perinatal mortality rates, although the study was too underpowered to detect this outcome. The expectant management group had a significantly higher rate of cesarean deliveries resulting from fetal distress, but there was no difference between groups in the rate of cesarean deliveries resulting from dystocia. The expectant management group had a significantly higher rate of cesarean deliveries than the induction group (odds ratio, 1.22 95 percent confidence interval, 1.02 to 1.45 number needed to induce to prevent one excess cesarean delivery, 30). 10 – 12 Expectant management continued until 44 weeks' gestation or until there was an obstetric indication for labor induction. Monitoring consisted of daily kick counts, nonstress tests (NSTs) three times per week ( Table 2), 9 and ultrasound amniotic-fluid–volume assessments two or three times per week ( Table 3). In this study, 3,407 women with pregnancies of at least 41 weeks' gestation were randomized to immediate induction or expectant management with fetal monitoring.
Placental abruption in a previous pregnancy that wasn't caused by abdominal trauma. Risk factorsįactors that can increase the risk of placental abruption include: Possible causes include trauma or injury to the abdomen - from an auto accident or fall, for example - or rapid loss of the fluid that surrounds and cushions the baby in the uterus (amniotic fluid). The cause of placental abruption is often unknown. Seek emergency care if you have signs or symptoms of placental abruption. Your baby might not grow as quickly as expected, and you might have low amniotic fluid or other complications. In some cases, placental abruption develops slowly (chronic abruption), which can cause light, intermittent vaginal bleeding. It's possible for the blood to become trapped inside the uterus, so even with a severe placental abruption, there might be no visible bleeding. The amount of vaginal bleeding can vary greatly, and doesn't necessarily indicate how much of the placenta has separated from the uterus. Uterine contractions, often coming one right after anotherĪbdominal pain and back pain often begin suddenly. Vaginal bleeding, although there might not be any. Signs and symptoms of placental abruption include: This study also included RCTs published after the most recent amendment to the Cochrane review.Placental abruption is most likely to occur in the last trimester of pregnancy, especially in the last few weeks before birth. In the other review, 2 the inclusion criteria were limited strictly to studies in which induction was initiated at 41 weeks' gestation or later. The benefit of induction was found in studies in which induction occurred after 41 weeks. Trials included in the Cochrane review 13 fell into two main groups: those in which women were recruited at or before 40 weeks' gestation and those in which recruitment occurred at 41 or 42 weeks' gestation. The primary difference between the meta-analyses was in the studies chosen for inclusion. In both reviews, the largest single RCT was the CMPPT (3,407 patients) the next largest individual RCT included 440 women. In neither review did an “unfavorable” cervix at the time of induction result in increased rates of cesarean delivery or other adverse outcomes. Neither review 2, 13 found any adverse perinatal complications from labor induction, and both noted that the results were consistent regardless of the Bishop score at the time of induction. No differences were found in neonatal morbidity outcomes. No difference was found in perinatal mortality rates, although the study was too underpowered to detect this outcome. The expectant management group had a significantly higher rate of cesarean deliveries resulting from fetal distress, but there was no difference between groups in the rate of cesarean deliveries resulting from dystocia. The expectant management group had a significantly higher rate of cesarean deliveries than the induction group (odds ratio, 1.22 95 percent confidence interval, 1.02 to 1.45 number needed to induce to prevent one excess cesarean delivery, 30). 10 – 12 Expectant management continued until 44 weeks' gestation or until there was an obstetric indication for labor induction. Monitoring consisted of daily kick counts, nonstress tests (NSTs) three times per week ( Table 2), 9 and ultrasound amniotic-fluid–volume assessments two or three times per week ( Table 3). In this study, 3,407 women with pregnancies of at least 41 weeks' gestation were randomized to immediate induction or expectant management with fetal monitoring. #LOW AMNIOTIC FLUID MEDICAL TERM TRIAL#
The Canadian Multicenter Post-term Pregnancy Trial (CMPPT) 8 is the largest individual randomized controlled trial (RCT) to date comparing labor induction at 41 weeks with expectant management. Elective labor induction before 42 weeks' gestation has been proposed to reduce rates of adverse fetal and maternal complications.





 0 kommentar(er)
0 kommentar(er)
